We are here to prepare for, and make sure that the surgery is done with the utmost safety at mind.
However, to have a blade pointed at the human body is in fact a very dangerous action.
During the surgery there is hardly anything that leads to trouble, but there is that certain probability that things that can not be predicted occur.
Amongst them, the ones that comparatively seem to occur easily are damage to surrounding organs, bleeding after surgery, infection, deep-vein thrombosis, and side-effects of the anesthesia to name a few.
In regards to damage to the surrounding organs, in cases of adhesion, damage occurs easily to intestines, bladder, urinary duct, and blood vessels.
Regarding post-operative bleeding, it may occur when the scar tissue (scab) of the hemostasis part comes off, or by when the thread used to stop the blood vessels comes off by stimulation.
Surgical wounds are weak to bacteria, and often infections occur from the indigenous bacteria of the skin and intestines, but originally, it occurs more easily in people with salpingitis and endometriosis and those with rupture of an ovarian cyst.
Deep-vein thrombosis causes organ damage when a blood clot (hardened blood) forms in the vein and that goes up into the lungs or the heart.
The frequency is low, but because there is a high fatality rate, at our clinic we are doing the treatment to lower the occurrence rate by having the patient wear elastic stockings.
Regarding complications of anesthesia, it may cause a severe headache during epidural anesthesia and spinal anesthesia, and by the reaction of the medicine.
Since the operating range is limited in surgery by the laparoscope, there is a tendency for complications being likely to occur.
In that case, due to safety we will change to laparotomy without hesitation.
In the case where it is difficult to support the complications at our clinic, there are times when we will be allowed to transport you to another medical facility.
It might not be called a complication, but after the operation for a certain amount of time there will be pain until the wound heals.
The pain, along with the recovery of the wound will gradually decrease.
Compared to be previously, the improvement of surgical treatment and various new medicines have been made and will continue to improve, but even so the pain can not be obliterated completely.
It is necessary to bare the pain for 1 day after the operation.
Also the period for hospitalization as compared to previously has become shorter.
Things like the improvement of surgical techniques and improvement of surgical materials are big, but it will take a certain amount of time for the wound to heal.
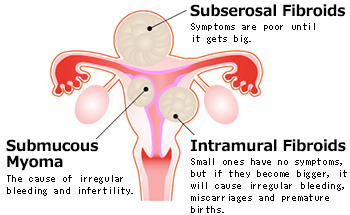
It is necessary to rest for about 1~2 weeks at home after being released for those who had the ovarian cyst surgery with no trouble in post-op.
2-3 weeks of rest is necessary for patients after release of myoma enucleation.
Additionally, in regards for those after having myoma enucleation, it will usually take about 6 months before you will be permitted to have a pregnancy.